Hippocampal Tail Volume as a Predictive Biomarker of Antidepressant Treatment
Author: Dr. Nikita Nogovitsyn
Editors: Dr. Sagar Parikh and Dr. Wegdan Rashad
Background
Imagine you wanted to predict which athlete might perform well in a weightlifting competition. One way you could try is to measure the size of key muscles in different individuals and see if bigger muscles correlated with success at lifting heavier weights. A similar approach can be applied to the brain that are involved in mood. If there is a part of the brain heavily involved in mood, can the size of that part tell us if the person can handle mood challenges better as compared to those individuals who have a smaller “mood muscle”?
One key part of the brain is the hippocampus, a structure that sits at the crossroads of all incoming information. The hippocampus plays a critical role in many aspects of emotional behavior and is also particularly involved in learning and memory. The hippocampus is composed of multiple layers, with each layer made up of unique brain cells (neurons) that have specific functions.
Some parts of this structure are particularly vulnerable to the adverse effects of stress. It has been previously shown that patients with a significant history of depression can have smaller volumes of the hippocampus tail than healthy controls. And the changes in the hippocampal tail in patients with depression may potentially inform about how successful the antidepressant treatment will be.
Study Question
In our newly published paper, we were interested in whether the hippocampal tail measurements can serve as a biomarker of antidepressant treatment. Biomarker is a biological measure (e.g. blood test, brain scan) that can be used to help clinicians distinguish between patients who will or will not respond to antidepressant treatment. In other words, would these brain measures have the capacity to predict clinical outcomes in participants with depression?
Study Groups
The CAN-BIND-1 study is looking for biomarkers of response to depression treatment. At the start of this study, we collected magnetic resonance imaging (MRI) brain scans from 196 patients diagnosed with major depression and 110 healthy comparison participants. Using these scans, we measured the volumes of several key brain structures, including the hippocampus and its parts, the size of brain ventricles, and the total brain volumes.
For the next eight weeks, participants with depression were treated with a commonly prescribed antidepressant drug, escitalopram. During the study, clinicians also measured the severity of depressive symptoms using the Montgomery-Asberg Depression Rating Scale (MADRS). Those patients who did not improve, as they did not report the severity of their depressive symptoms dropped by 50%, were prescribed additional medication, aripiprazole, which they took for another eight weeks. If signs and symptoms of depression disappeared (at least in part) – these patients were called remitters.
At the end of the study, following 16 weeks of medication use, patients were split into three major groups.
- Non-remitters: patients who were not relieved from depressive symptoms at any point in the study.
- Late remitters: patients who remitted only by the end of the study (by week 16).
- Early remitters: patients who were relieved from most of the depressive symptoms by week eight using a single antidepressant.
Study Results
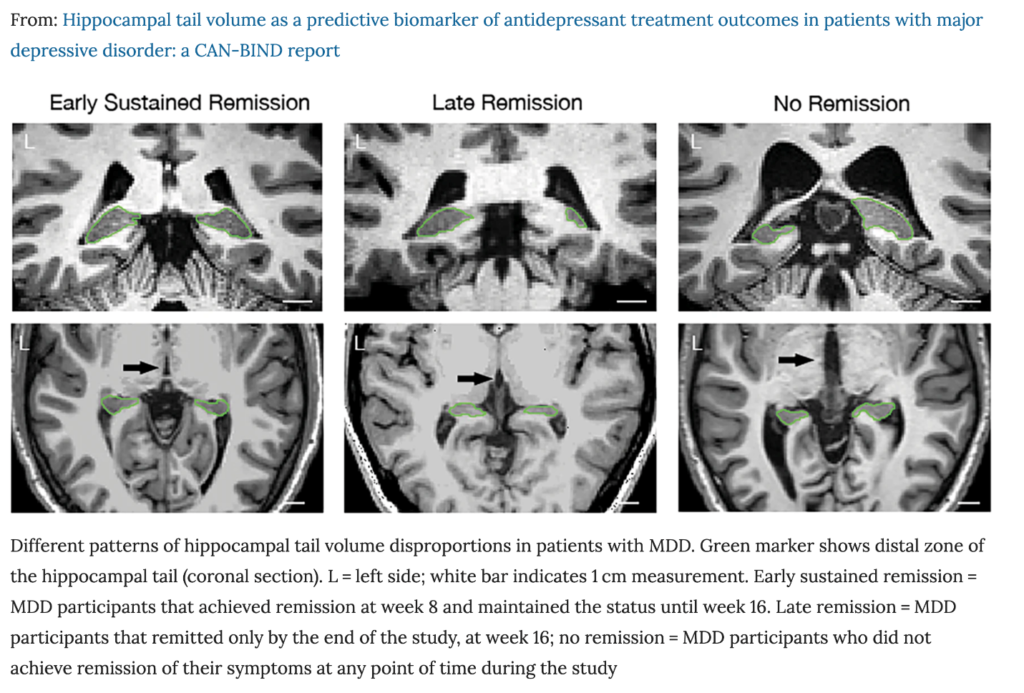
We analyzed MRI scans from all participants collected at the beginning of the study and found that brain images from three patient groups looked different. Specifically, non-remitters had the right hippocampal tail larger than the left one. In addition to this, non-remitters showed disproportionally larger ventricle sizes relative to the hippocampus. Although late remitters did not have disproportionally large ventricles, they displayed a greater volume of left hippocampal tail than the right one. Finally, early remitters did not have any detectable brain volume disproportions or asymmetry in the hippocampal tail. These comparisons suggested that disproportionally small hippocampal tail volumes can inform us about poor treatment outcomes.
Conclusions
Therefore, our study results show that the degree of hippocampus tail disproportion measured at the start of the treatment may predict both the rate and likelihood of successful antidepressant treatment. Although we don’t completely understand the mechanisms connecting brain changes and clinical outcomes, hippocampal tail volume measurement appears to be an informative biomarker for antidepressant medication therapy. In terms of the next steps, future studies should try to replicate these findings and test whether hippocampal tail disproportions can inform about clinical outcomes following other treatment approaches, including psychotherapy and a combination of various types antidepressants.
References
Nogovitsyn, N., Muller, M., Souza, R., Hassel, S., Arnott, S. R., Davis, A. D., … & Ismail, Z. (2020). Hippocampal tail volume as a predictive biomarker of antidepressant treatment outcomes in patients with major depressive disorder: a CAN-BIND report. Neuropsychopharmacology, 45(2), 283-291. https://www.nature.com/articles/s41386-019-0542-1