Deciphering the Relationship Between Brain Structure and Epigenetics in Depression
Author: JeeSu Suh, BSc (Ph.D. Candidate in the Graduate Neuroscience Program, St. Joseph’s Healthcare, Hamilton)
Editors: Dr. Wegdan Rashad Abdelmoemin, Dr. Sagar Parikh, and Mr. Andrew Kcomt
Background
Stress can cause depression which in turn triggers immune and hormonal responses in the brain and body. This response is designed to optimally prepare you for stressful situations, whether they be physical, social, or emotional. Throughout the course of human evolution, it was designed to be a brief response that dies down quickly once the stressor passes. But in our modern world, our stressors might include things like debt, precarious employment, prolonged interpersonal conflict, or feelings of exclusion at work, among others. These problems are not easily or quickly resolved, and in some people, the stress response never turns off, and depression can ensue.
The hypothalamus is a small region of the brain nestled under the cerebrum (the large, folded part of your brain) at the level of your eyes. It starts and controls the stress response via a series of hormonal actions, turning it off once no longer needed in normal situations. In depression, this regulation is compromised. Interestingly, the hypothalamus also regulates sleep, appetite, sexual behaviour, and a host of other basic bodily functions that are also affected in depression. However, research on the hypothalamus in living humans has fallen behind work on other brain regions, mostly because it is difficult to visually define in brain scans.
Another piece of the puzzle has to do with epigenetics. Epigenetics is the study of how the environment we live in can affect our genetic functioning. In that sense, epigenetics represents the interaction between nature and nurture, where genes (and the hormones they encode) may be turned “on” or “off” with external modifications. A common modification is the reversible addition of a chemical group (called methylation) to specific locations on DNA to regulate gene activity. Therefore, it is reasonable to predict that the activity and abundance of stress hormones might be affected by epigenetic modifications. Up to this point, very few studies have studied holistic links between brain and epigenetic factors in depression.
Study question
- Are hypothalamus volumes in depression related to the epigenetic profiles of 3 key stress hormones?
- Is depression and its clinical characteristics related to hypothalamus volumes?
Study groups and plan
Using brain scans from 181 individuals with current depression and 90 healthy control participants, we manually traced the hypothalamus and calculated its volume for each brain, which is currently the gold standard for accurate segmentation of this region.
We created 4 models in total, dividing the hypothalamus into right and left volumes, and within each participant group:
- Left hypothalamus volume & epigenetics in currently depressed participants
- Right hypothalamus volume & epigenetics in currently depressed participants
- Left hypothalamus volume & epigenetics in healthy participants
- Right hypothalamus volume & epigenetics in healthy participants
Study results
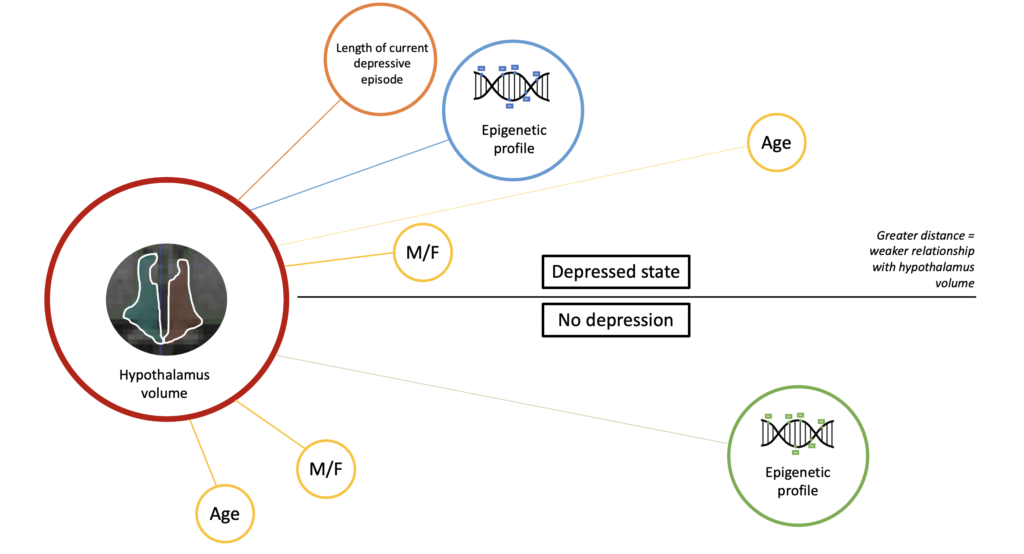
First, we demonstrated that sex and age are significant factors affecting hypothalamus volume in both groups. There was a modest relationship between longer episode duration and smaller volume of the left hypothalamus. In healthy participants, the reference variables of sex and age were more associated with hypothalamus volume than epigenetic profiles of stress genes, indicating a weak relationship between brain and epigenetics in the healthy state.
However, in the currently depressed individuals, a much larger number of epigenetic profiles ranked higher than age, which was already shown to be significantly related to hypothalamus volume. In addition, the epigenetic profiles at 2 of these locations were related to gene expression, indicating they have a role in stress gene regulation. These two DNA locations have already been identified in previous studies to be related to PTSD symptoms and cortisol reactivity, further validating this finding.
Conclusion
We found a stronger connection between hypothalamus volume and epigenetics of stress genes in the currently depressed state that was not observed in healthy individuals. Although we can’t say in which direction this connection flows due to our single-timepoint design (does hormonal stress dysregulation affect hypothalamus volume or does hypothalamus volume alter regulation of stress genes?), this result takes us a step closer to untangling the threads of the molecular and neural chaos that characterizes major depression.
Reference
Suh, J.S., Fiori, L.M, Ali, M., Harkness, K.L., Ramonas, M., Minuzzi L., Hassel, S., … & Frey, B.N. (2021). Hypothalamus volume and DNA methylation of stress axis genes in major depressive disorder: a CAN-BIND study report. Psychoneuroendocrinology, 132(105348). https://www.sciencedirect.com/science/article/pii/S0306453021002225
Published: 09 Aug 2021